Distant Diagnosis
by Christopher Vaughan *
1.20.04 -- Avin Brigman leads a pretty quiet life, an average life. The 32-year-old welder lives with his wife and two children just two doors down from his parents in Imperial, California, a small town 111 miles east of San Diego. But when a blood clot lodged in his brain during a midday walk in August, he became a horrible exception, a young man whose life was suddenly jeopardized by a stroke.
Brigman's ordeal began as he was walking to his parents' house and felt a "bad headache" coming on. He'd had migraines before and thought this was just the beginning of one more head-splitting attack. This time, however, he began feeling numb along his right side. "Like most guys I just thought it would go away," Brigman says, "but when I couldn't move my arm at all I began to think that something must be really wrong."
Arriving at his parents' house, Brigman called his wife. She listened to his symptoms and insisted he go to the hospital. By the time they had driven the 10 miles to Pioneer's Memorial in nearby Brawley, Brigman was paralyzed along the whole right side of his body-a major indicator of stroke.
|
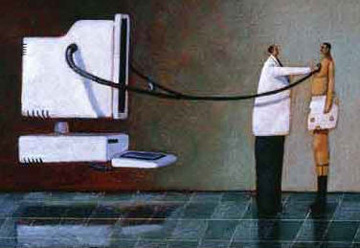
At the hospital, however, he became exceptional in a lucky way. The emergency room doctors were able to confirm the stroke diagnosis quickly enough to give Brigman a new medication that dissolves blood clots and restores blood flow to oxygen-starved brain cells. The doctors used StrokeDoc, a newly developed audiovisual link that connected them with stroke specialists at UCSD.
The fruit of a marriage between UCSD's expertise in both cell phone engineering and stroke research, StrokeDoc has broken the vexing rigidity that shackled the practice of medicine over an audiovisual hookup. Until now the fixed point-to-point nature of a dedicated wire going from one base station to another has limited the scope of telemedicine. The flexibility of mobile connections vastly increases the efficiency of telemedicine and has the potential to change the way strokes are treated.
Getting a complete diagnosis in a timely manner is important in all emergency medicine, but especially in dealing with stroke. Since 1996, a natural clot-busting enzyme called tPA (thrombolytic plasminogen activator) has been astoundingly successful in treating strokes caused by blood clots. It has vastly improved the odds that patients will survive a stroke with minimal disabilities.
Exciting though that prospect is, tPA has major drawbacks. There are two kinds of stroke, and if tPA is used to treat one caused by bleeding into the brain rather than one caused by a blood clot, the drug will increase the bleeding and result in more brain damage or even death. The other drawback is that tPA has to be administered quickly-within three hours of the onset of symptoms. Studies have shown that, after that time, tPA doesn't help the brain cells affected by the stroke.
Physicians at local hospitals are therefore understandably wary about using tPA without a thorough evaluation by a stroke specialist, and they are unlikely to administer the drug if such a diagnosis is delayed. Stroke specialists may not be on staff or on duty when patients are brought into smaller hospitals; therefore many patients miss the three-hour window.
"Looking at the data, it is clear that there is a problem," says Patrick Leyden, head of the neurology department at UCSD and one of the principal investigators on the original study of tPA conducted by a consortium of medical centers, one of which was UCSD. "The studies have shown that 2 to 5 percent of stroke patients are getting this drug, but the numbers should be more like 30 percent."
These percentages translate into enormous human suffering and disability. Stroke is the third leading cause of death (after heart disease and cancer) and the leading cause of disability in the United States, afflicting about 700,000 Americans every year.
It was clearly not possible to get every stroke patient to a specialist within three hours, so Leyden saw only one solution: bring the specialist to the patient, via telemedicine. Doing so, however, would require a vast improvement in technology.
In a sense, telemedicine has been around ever since a doctor made the first diagnosis over the telephone. But the term has only been in use since doctors started using interactive audiovisual systems. These systems allowed patients and physicians to see and hear each other even though they were separated by thousands of miles. The limitation was that they had to be hardwired from one telemedicine base station to another.
"In regular videoconferencing both parties are at the end of a single, dedicated wire, so the doctor has to be on one end of the wire at a TV console and the patient has to be at the other end," Leyden says. Getting each party to these fixed ends of the wire often proves almost as difficult as getting a stroke expert to the patient on time.
Leyden needed a more flexible system. Something that could reach patients and doctors anywhere. Like a cell phone. Luckily enough, San Diego is home to some of the biggest cellular technology companies in the world, and UCSD has some of the most accomplished cellular experts on its faculty. Leyden approached Ramesh Rao, a professor of electrical engineering at the Jacobs School of Engineering and director of the UCSD division of the California Institute for Telecommunications and Information Technology-known as Calit2. He told Rao that they needed to replace their current system, which was to have a physician jump in a car and race to one end of a fixed-wire TV console at the hospital.
Making such a replacement proved more difficult than Rao first imagined. "The features and the quality of the system that the physicians were asking for turned out to be quite demanding," he says.
Leyden was asking for a camera that could be controlled remotely so that the distant stroke expert could pan and zoom the lens. That way the neurologist could look at what he wanted, just as if he were in the room. In addition, the camera would be connected to a laptop that could go anywhere and would connect instantly via a cellular connection with another laptop. Either laptop might be in an airport, at a hospital, or on the golf course.
"The physicians of course don't like it when people use the golf course example," Rao quips. "They prefer to talk about using the system when they are stuck in traffic."
The data transmission requirements of the system were the most demanding of all. "The existing software out there was geared toward transmitting video clips, which are often quite grainy," Rao explains. In order to get the kind of video quality necessary for a correct diagnosis, physicians needed a data transmission rate of 10 megabits per second on the existing hardwired telemedicine systems. Using a cellular system would demand compressing the same quality substantially. "We wanted to get that down to one megabit per second," Rao says.
This part of the challenge was met through a collaboration with Path 1 Network Technologies, a company that had been independently developing a system to transmit DVD quality video over a cellular network. The chief technology officer of Path 1, Ronald Fellman, was a professor of electrical and computer engineering at UCSD from 1988 to 1996.
In addition to extensive connections between the University and the cellular industry, UCSD also has an FCC license for a cellular base station on campus, something that is important in building a telemedicine cellular network. "We have a cellular communications infrastructure that is truly one of a kind," Rao says. "Usually these base-station licenses are owned by commercial companies like Verizon or Sprint."
Rao's group, in collaboration with private industry, ended up developing entirely new software for encoding and transmitting high quality video images, software that is not yet commercially available. The final application utilizes University and commercial cell systems, as well as the Internet, to get the images from one laptop to another. "This wasn't just bundling together commercial applications. We had to go out and develop entirely new ways of doing things," Rao says. "The key innovation was managing errors on the wireless links ...since these links are notoriously prone to error." Rao and his group therefore created a system that allowed three seconds to run more sophisticated error recovery algorithms and retransmit those packets that had been received in error.
Although the effort involved was immense, Leyden and Rao say the payoff will be worth it. Once high-quality video and audio are available via any cellular connection, telemedicine could be used for all sorts of emergency applications beyond stroke therapy. "There are a lot of fields, such as critical care and cardiology, where there are severe time constraints" on getting the patient expert care, project director Brett Meyer says.
Once they are freed from a dedicated, point-to-point system, UCSD physicians might find themselves providing expert advice for patients in Anaheim, Arizona or Angola. Rural areas of the United States that now go begging for qualified general practitioners would have access to the best specialists in the field.
"The way doctors take care of stroke patients today around the country is based in part on research done at UCSD over the last 15 to 20 years," Leyden says. "In the same way, if we are successful, this methodology will be diffused throughout our country and throughout the world."
Once the system is widely available, physicians at major medical centers will be able to deliver their expertise anywhere it is needed, if there is a cellular signal. If a train or airliner crashes in Helena, Montana, for instance, critical care physicians from around the country will be able to chip in and help triage patients, then offer advice to local doctors on their care. A physician on an Indian reservation or in an Appalachian hollow, who might miss a diagnosis of dengue fever because he's never seen it, could instantly get a second opinion from the foremost tropical disease experts in the country. The applications are almost limitless. "Whenever physicians see what we have developed they say, 'We've got to have one of these,'" Meyer says.
It took two years of work by UCSD physicians and engineers, toiling side by side, to iron out the problems in the new system. Once the technical difficulties were solved, it was time to test the system. "We strapped a digital camera to a laptop with bungee cords and made this little prototype," Rao says. "Pat Leyden liked it." Shortly thereafter, Leyden and project director Meyer began placing the new cellular telemedicine stations in five hospitals, as part of a scientific study of the system's effectiveness. Pioneer's Memorial in Brawley was the first hospital to get one, just in time to save Davin Brigman.
Emergency room physicians suspected stroke immediately when Brigman came in, due to the complete paralysis on only one side of his body. They quickly did a CT scan of his brain and then brought in the StrokeDoc hookup. "They rolled in a cart with a flat-screen computer and a camera, and told me I would be talking to a doctor at UCSD," Brigman says. Although Brigman thought it strange to be examined by a computer, he felt it was no stranger than everything else that had happened to him that afternoon. "It actually was like he was right there," Brigman says of Meyer. "He could see me and knew what I was doing, and there was no delay."
Within one hour of the initial headache, the doctors in Brawley were administering tPA to Brigman. By the time he was on a helicopter to UCSD's Stroke Center that evening, he started to feel better.
Weeks after the stroke, Brigman says almost all his functions have returned, except for his sense of taste. "I still can't taste anything, so I tend to eat too much," he says.
Still, Brigman knows how lucky he is. If his stroke had come even a couple of months earlier he might never have been given tPA and might have ended up with severe disabilities despite the best efforts of the doctors in Brawley. Had this happened, Brigman would have merely been repeating the experience of thousands of other stroke victims in small towns across America.
That's a reality that UCSD scientists hope to change. "This technology brings us one step closer to helping people who we have never been able to help before," Meyer says.
# # #
*Christopher Vaughan has written numerous books and articles on biomedicine. He lives in the San Francisco Bay Area. This article is reprinted from the inaugural January 2004 issue of @UCSD magazine, published by the UCSD Alumni Association.